Why Has Israel Succeeded At COVID Vaccination?
Israel has pulled ahead of much in the world in its rate of vaccinating its citizens - with roughly 1% of the entire population vaccinated per day and over 23% of the country vaccinated in the first few weeks. The country hopes to have the entire population over age 16 vaccinated for COVID by end of March.

Israel focused on first vaccinating people by age group (and then comorbidity) with the idea that if you vaccinate the 20% of the country that represent 95% of the deaths, you can avoid deaths from COVID.
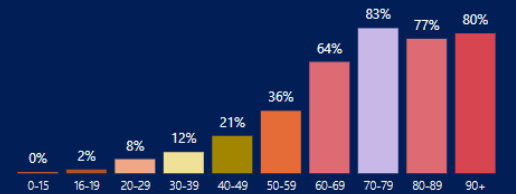
% of Israeli population within a certain age vaccinated by 1/13/21. Chart via Segal Eran
Early data is starting to suggest Israel’s approach is working. For example, in a cohort of 200,000 people vaccinated in Israel, there was a 12X drop in COVID cases by day15-22 of a single dose of Pfizer/BioNTech vaccine.
The right hand column below is day since first shot to result. The left hand side is # positive for COVID.

In parallel much of the rest of the world has been slower on rolling out vaccination with UAE as an exception.
After speaking to a number of members of the Israeli public health community involved with COVID, the following picture emerges on why Israel has been so successful:
1. Focus on simplicity & pragmatism.
The biggest takeaway is a focus on simplicity and pragmatism. For example, the criteria for vaccination are simple - you are either a healthcare worker (including nursing homes & assisted living facilities), or you are tiered by age (and later comorbidity).
Healthcare workers have been shown to spread COVID and other diseases within hospitals (known as “nosocomial transmission” and a key aspect of SARS and MERS - two other coronavirus based diseases), while older people are most vulnerable to hospitalization and death from COVID.
Having age-based tiers makes it easy to know who should show up and who is eligible, and removes a big burden on enforcement.
This simplicity and pragmatism extends further. For example, in the USA the roll out of vaccination in California to healthcare workers was slowed by complex tiering within healthcare workers themselves based on how much patient facing time each type of workers has.
In contrast, the Israelis I spoke to said “We vaccinate an entire workplace. We assume everyone will eventually be vaccinated so we found it easier to just show up and vaccinate every single person who works at a hospital. We do not care if they are doctors or administrators or whatever - it is easier to just vaccinate everyone”.
Many countries and states have been too focused on “fairness” and “equity” so have frozen their vaccination efforts in place, or put in place large fines for “misused virus”. Remember - everyone will eventually get vaccinated. The more shots in arms, the better, with an emphasis on the old and comorbid. And also remember, we are in the middle of a “once in a century pandemic”- it is more important to move fast to save lives than to create and enforce complex rules. However, it turns out these complex rules are not needed - there are simple criteria for who will get sick and die of COVID per below.
2. Vaccinate the people who will die.
The biggest risk factor for death and hospitalization from COVID is age. Age outweighs comorbidities in some cases by as much as 30-fold. A handful of comorbidities matter, but age dominates.


Simple math suggests that vaccinating roughly 20-25% of the population would prevent 95% of COVID deaths in many western countries. So, pragmatically, the Israelis focused on vaccinating that high-risk 20% of their population first. This has mapped to age-based tiers (and a handful of comorbidities) which simplify vaccination roll outs. They also vaccinated healthcare workers and long term care facilities first.
Many of the calls in the US for “ethics and equity” in vaccination seem to be politically motivated versus science based. Complex, multi-tier criteria that prioritize young “essential” workers over 70-year olds, who are much higher risk of dying of COVID, means more people will die as we wait to get to the 20-25% of the population who actually matter in terms of risk of hospitalization and death. There is little logic in vaccinating 30-50% of the population (depending on your definition of "essential workers") and then 20% of high risk people (50-70% of the entire population between them!!) to protect 20% of the population who contribute 95% of COVID deaths. It is much easier to focus on the 20-25% who are actually at risk first. It seems unlikely it is ethical, or equitable, to let people die for your “ethics & equity framework”.
The science is clear - vaccinate the elderly, then people aged 16+ with certain comorbidities and you will see COVID deaths plummet. (Side note, the CDC finally updated their criteria to 65+ while this document was being written). We should all honor the role essential workers have played in keeping the country and world open. One way to honor this is to protect their elderly and sick family members from dying of COVID - by vaccinating their at-risk family members first. After the people with highest risk of death are vaccinated, the subset of essential workers who did not fall under those demographics can be vaccinated next. For example, Israel started this week vaccinating 55-year olds and up, as well as all teachers.
The nice aspect of this approach is you do not need to vaccinate that large of a population before you see a big impact and can potentially reopen. If fewer people will die of COVID (once vaccinated) then other common diseases like flu going forward, a country or state can reopen with many lives saved.
Here is Israel’s prediction on what to expect in terms of deaths:

3. Create as many endpoints to vaccinate out of as possible.
The Israelis I spoke to emphasized their focus on opening as many vaccination clinics and centers as possible. They mentioned that when a hospital set up a vaccination program, every possible clinic in the hospital was also opened for vaccination.
Similarly, parks, schools, and other public spaces have been converted into places people can go to be vaccinated.
Israel has also opened some “mega centers” for vaccination, per the picture below.

Some cities like San Diego have recently followed suit after feeling stymied by State and Federal government:

4. Don’t waste vaccine.
Remember, everyone will eventually be vaccinated. Throwing a scarce vaccine in the trash is an enormous waste. Rather than waste vaccines, the Israelis have two mechanisms for overflow. First, anyone can wait in line by a vaccination center starting at 7pm and if there is vaccine left over, be vaccinated. Second, if no one is waiting in line nurses or other vaccinators will go out into the street looking for people to vaccinate (and then schedule their next appointment for the second dose on the spot). There is a famous story of nurses coming out of a clinic and spotting a pizza delivery person. “Hey pizza guy want a vaccine!!” they yelled to call him over and then vaccinated him.
5. Success begets success.
Israel has been incredibly transparent on data around the vaccination program - with everything from dashboards showing vaccines used per day, % of population by age vaccinated etc. to a Telegram channel from the Ministry of Health with daily data dumps to whomever signs up.
One general tenet of life is “success begets success”. By vaccinating rapidly the pharma companies approved in Israel (Pfizer and Moderna) have continued to prioritize the company for more vaccine as capacity comes online. While Israel originally expected a gap in deliveries and temporarily running out of vaccine in January, that gap has now been bridged via new pharma deals.
The US could consider doing something similar - allocate more vaccines to the states that are actually using it. Hold back vaccine from states that are not moving quickly until they move fast enough to use it.
Remember - we do not need to vaccinate everyone to have a big effect. If we vaccinate 20% of the population it might be possible to still drop deaths 95%, which is the primary goal of the COVID shelter-in-place, social distancing, and vaccination efforts.
Factors that are mentioned but seem overweighted (AKA excuses).
There are a lot of reasons (perhaps a better word is “excuses”) that are made for why Israel is succeeding while others are not. This includes things like:
a. Small population and geography.
Israel is a country of 9 million people. The argument is its small size makes it easier to vaccinate. The reality is that many countries the same size or half the size of Israel are doing a much worse job of vaccinating their populations including Denmark (5 million), Norway (5.3 million), Netherlands (18 million) and others. Similarly, States like New Jersey (population of ~9 million) are far behind Israel as well. If size were the only constraint, we would see more success elsewhere.
b. HMO/healthcare centralization.
The Israeli population is largely covered by 4 HMOs - with the largest, Clalit, covering roughly 50% of the population. Centralization of healthcare services undoubtedly matters in decision making speed and administration. However, as reminder the fragmented US system vaccinates 50% of its entire population age 2 and up for flu every single year - and does so in a matter of weeks. The primary obstacles in the US seem to have less to do with centralization and more with complex criteria and fears of scarcity of vaccines driving even more scarcity.
c . It must be the Israeli military coordinating all this!
The Israeli military is not coordinating the population’s vaccination. It is driven by a combination of the Ministry of Health, the HMOs, and some private companies that have been contracted for a subset of the logistics. This is all do-able in the USA too.
d. Israel is a wealthy country! That must be why! Or they spend more on healthcare!
Israel GDP per person is lower than the USA overall as well as lower than states of the same size like New Jersey. The country also spends around 7% of GDP annually on healthcare - roughly one-third what the USA spends.
e. The culture is different!
Israel has more in common with the US than one might guess. There is a fractured, contentious political system. A number of healthcare workers were going to refuse the vaccine - until they were told they would be placed on administrative leave if they refused it. A meaningful subset of the population ignored their second lockdown.
The USA can do it too!
Every year the United States vaccinates 50% of its entire population over the course of a few weeks for the flu. In past outbreaks the country has also been fast to move. For example, in 1947 the city of New York vaccinated 5 million people in 2 weeks to combat a smallpox outbreak.
If needed, the country can move fast. In order to do so, it should:
(1) Simplify criteria. Make vaccination age-based (and include healthcare workers and assisted living facilities). Be pragmatic. Vaccinate the whole hospital versus quibbling on the order in which staff get it. Remember - everyone will eventually be vaccinated. The two goals are to stop deaths and then to build herd immunity - in that order.
(2) Focus on the people who will actually die of COVID, not politics. 20-25% of the population vaccinated may drop deaths 95%. The CDC is finally moving in this direction, but should focus on age-based and then co-morbidity based tiering versus other factors. “Fairness” falls out naturally if everyone is vaccinated in the next few months and everyone’s family members’ lives are saved, versus taking an entire year with incremental disease and deaths.
(3) Open as many vaccination points as possible as fast as possible.
A simple model is that anywhere that administered the flu vaccine can be used to vaccinate for COVID. Or, augment the pop-up testing centers with vaccination services. These stations can be staffed by healthcare workers from the clinics being used, as well as pharmacists (trained in flu vaccination), dentists and others.
(4) Don’t waste vaccine. If there is excess left over, use it on anyone so we can build herd immunity faster.
(5) Optional - reward success. If a city,region, or state moves extra fast at vaccination - give them more. Reward the communities that vaccinate quickly and create competition and a leaderboard to get it done.
We finally have a vaccine. Many people are now dying unnecessarily due to a lack of delivery. The Israel model suggests a clear way to move forward. Let’s get it done.

